Guest Blog:
KelaHealth is pleased to present this guest blog by Douglas Slakey, MD, MPH, Chief of Surgical Services at CMC Advocate Aurora Health. Here, Dr. Slakey answers our questions about using artificial intelligence (AI) and machine learning methods to identify risk factors and optimize patients prior to surgical care.

How does a surgical care team evaluate a patient for surgery?
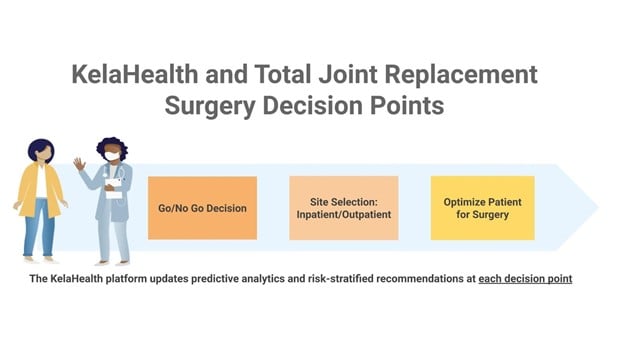
Surgical care teams evaluate a number of factors when determining whether and when to operate on a patient. Each individual is unique, and a number of variables impact a patient’s readiness for surgery. In particular, patient risk factors, which are existing health conditions and health-related issues that may affect a patient’s likelihood of complications, are examined and used to inform clinical care.
What are some types of patient risk factors and how do they impact clinical care?
Surgical patient risk factors can be categorized into three broad, but interrelated categories: physiologic, genetic, and social determinants of health (SDOH). Physiologic factors such as obesity, poorly controlled diabetes, and frailty are well documented as increasing surgical risk, yet are inconsistently addressed by surgical teams or primary care physicians prior to elective surgery. Genetic risk factors may be self-evident or obscure but are undeniably important contributors to outcomes. SDOH, such as socioeconomic status, home support, transportation, education level, and language barriers, can also impact surgical risk, and may in fact exacerbate certain physiologic and genetic risk factors.
How do social determinants of health (SDOH) factor into the equation?
SDOH are known to significantly impact surgical outcomes; however, no consistent mechanisms exist to address them pre-operatively. Techniques available today to understand risk are a combination of individual knowledge and experience – both of which are subject to bias and limitations due to information available at the point of care. Admittedly, there are “risk calculators'' available. Most of these tools are based on retrospective analysis of patient outcomes using traditional statistical techniques and therefore may or may not be applicable to a patient currently being considered for surgery. Furthermore, the traditional surgical risk calculators do not include SDOH. This poses significant limitations. Consider two patients being considered for the same surgery. Both are diabetic, take the same dose of insulin, and have the same hemoglobin A1c. The risk calculators would indicate both have the same surgical risk. But let’s suppose one patient is from a college educated household with lots of support and the other is single, living in public housing without reliable transportation. Clearly each of these patients has a different set of risks related to surgery, but unfortunately the “traditional” surgical risk calculators would not provide this insight.
How is current patient risk assessment conducted?
At the current time, patient-related surgical risk assessment relies upon individuals – doctors and other members of the healthcare team. Arguably, this is not efficient and introduces a high degree of variability that is inevitable when the individual is held uniquely responsible without a system to support the decision-making. Tools such as lists to help guide questioning of patients and review of the EHR databases do exist; however, they are rarely used in practice due to time and other constraints. Most often, patient risk factors are simply listed within the medical record but are not modified prior to surgery, which is a missed opportunity to take the most optimized patient to surgery.
What efforts have been tried to date to address this?
Over the past decade, the belief that surgically relevant patient risk factors could not be comprehensively addressed has been challenged. For example, enhanced recovery after surgery (ERAS) protocols have demonstrated the benefits of optimizing surgical care by ameliorating physiologic consequences of surgical stress. Surgery as a discipline has taken significant steps to shift from the outdated paradigm of managing surgical patient complications after they occur (focusing on rescue), to actively trying to minimize the occurrence of complications.
What is Pre-Surgical Optimization and how is it different than what has been done before?
Pre-Surgical Optimization (PSO) is a comprehensive approach to optimizing patients, ensuring that they are holistically prepared for surgery. PSO can and should address many risk factors that impact surgical patient outcomes, such as medical diagnoses and co-morbidities, malnutrition, frailty, dementia, and social determinants of health (SDOH). PSO is a relatively new concept. PSO is an extension of enhanced recovery after surgery (ERAS) and strengthens the effectiveness of enhanced recovery programs – ideally the two are considered as part of the whole, the surgical home. Results reported in the literature(1-3) demonstrate that PSO can, amongst other things, reduce morbidity, reduce length of stay, readmissions, and cost, and improve satisfaction. These factors indicate that an effective PSO program will improve reliability, safety, and value in elective surgery. Not unexpectedly, we can expect that the greatest improvement in outcomes and cost savings realized by PSO would be in the highest risk patients.
Creating value in surgery requires a high reliability process in which modifiable and non-modifiable patient risk factors are recognized, understood, considered, and - wherever possible - addressed before the patient enters the operating room. This is a shift from traditional norms where adverse surgical outcomes were often attributed to “patient factors” considered inevitable and uncontrollable. In the traditional surgical paradigm, emphasis is largely placed on managing complications after the fact, an approach that limits efforts to increase reliability from both the individual surgical patient and population standpoint.
What can be done now to personalize surgical care and make surgery safer and more equitable for each patient?
We are at a point in time where we can, and should, use artificial intelligence (AI) and machine learning algorithms to support identification of risk and subsequent decision-making. Applying predictive modeling to determining which patients have significant surgical risk factors (physiologic, genetic, and socioeconomic) and to facilitate referral to surgical optimization will improve reliability, outcomes, and value.
The future for surgeons and others caring for surgical patients will be transformed as data is provided to them in a manner that accounts for the complex interplay of risks unique to each individual patient in a way that augments their ability to perform – enhancing human performance. The effective use of big data analytics delivered at the point of care is analogous to the heads-up display of a modern fighter jet. A series of data feeds that would be in and of themselves overwhelming and uninterpretable, are instead provided in a way that understands individual risks and facilitates decisions, providing the greatest confidence to the surgeon, the healthcare team, and the patient. Making this a reality will undoubtedly transform the way care is provided in a positive, humanistic manner.
Literature Cited
-
Desebbe O, Lanz T, Kain Z, Cannesson M. The perioperative surgical home: An innovative, patient-centred and cost-effective perioperative care model. Anaesth Crit Care Pain Med. 2016 Feb;35(1):59-66. doi: 10.1016/j.accpm.2015.08.001. Epub 2015 Nov 21. PMID: 26613678.
-
Elhassan A, Elhassan I, Elhassan A, Sekar KD, Cornett EM, Urman RD, Kaye AD. Perioperative surgical home models and enhanced recovery after surgery. J Anaesthesiol Clin Pharmacol. 2019 Apr;35(Suppl 1):S46-S50. doi: 10.4103/joacp.JOACP_47_18. PMID: 31142959; PMCID: PMC6515720.
-
McDonald SR, Heflin MT, Whitson HE, Dalton TO, Lidsky ME, Liu P, Poer CM, Sloane R, Thacker JK, White HK, Yanamadala M, Lagoo-Deenadayalan SA. Association of Integrated Care Coordination With Postsurgical Outcomes in High-Risk Older Adults: The Perioperative Optimization of Senior Health (POSH) Initiative. JAMA Surg. 2018 May 1;153(5):454-462. doi: 10.1001/jamasurg.2017.5513. PMID: 29299599; PMCID: PMC5875304.